Lbd Movie
On this page:
- In a single scene, she defined one of fashion's most iconic garments: the little black dress (aka LBD). British actress Audrey Hepburn on the set of Breakfast at Tiffany's based on the novel.
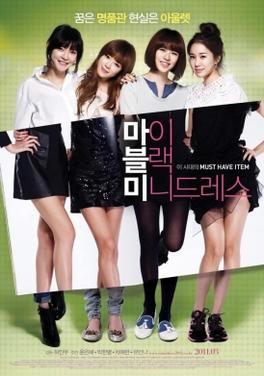
- Directed by In-mu Heo. With Eun-hye Yun, Han-byeol Park, Ye-ryeon Cha, In-Na Yoo. After graduating from university a group of five close friends have to define their own lives in ways that challenge their friendship.
- When does something unattainable set you on your course in life? Yoo Min (Yoon Eun Hye) is a 24-year-old woman who still doesn’t know what she wants to do in life. But when she sees an expensive little black mini-dress at a luxury department store, she knows she has to have it even though she can’t afford it. She uses the credit card of a famous writer to buy the dress, and as a result.
Lewy body dementia (LBD) is a disease associated with abnormal deposits of a protein called alpha-synuclein in the brain. These deposits, called Lewy bodies, affect chemicals in the brain whose changes, in turn, can lead to problems with thinking, movement, behavior, and mood. Lewy body dementia is one of the most common causes of dementia.
The first major film about a person with Lewy body dementia (LBD), Robin’s Wish tells the story of what people with this devastating disorder are really struggling with. Explaining the movie’s title and Williams’ main “wish,” Schneider Williams said the Oscar winner “wanted to help all of us be less afraid.”.
Diagnosing LBD can be challenging. Early Lewy body dementia symptoms are often confused with similar symptoms found in other brain diseases like Alzheimer's or in psychiatric disorders like schizophrenia. Also, Lewy body dementia can occur alone or along with other brain disorders.
There are two diagnoses of LBD—dementia with Lewy bodies (DLB) and Parkinson's disease dementia. The earliest signs differ but reflect the same biological changes in the brain. Over time, people with dementia with Lewy bodies or Parkinson's disease dementia may develop similar symptoms.
Lewy body dementia affects more than 1 million individuals in the United States. Lewy body dementia typically begins at age 50 or older, although sometimes younger people have it. LBD appears to affect slightly more men than women.
Lewy body dementia is a progressive disease, meaning symptoms start slowly and worsen over time. The disease lasts an average of 5 to 8 years from the time of diagnosis to death, but the time span can range from 2 to 20 years. How quickly symptoms develop and change varies greatly from person to person, depending on overall health, age, and severity of symptoms.
In the early stages of Lewy body dementia, symptoms can be mild, and people can function fairly normally. As the disease advances, people with LBD require more help due to a decline in thinking and movement abilities. In the later stages of the disease, they often depend entirely on others for assistance and care.
Some Lewy body dementia symptoms may respond to treatment for a period of time. Currently, there is no cure for the disease. Research is improving our understanding of this challenging condition, and advances in science may one day lead to better diagnosis, improved care, and new treatments.
What are Lewy Bodies?
Lewy bodies are named for Dr. Friederich Lewy, a German neurologist. In 1912, he discovered abnormal protein deposits that disrupt the brain's normal functioning in people with Parkinson's disease. These abnormal deposits are now called 'Lewy bodies.'
Lewy bodies are made of a protein called alpha-synuclein. In the healthy brain, alpha-synuclein plays a number of important roles in neurons (nerve cells) in the brain, especially at synapses, where brain cells communicate with each other. In Lewy body dementia, alpha-synuclein forms into clumps inside neurons, starting in areas of the brain that control aspects of memory and movement. This process causes neurons to work less effectively and, eventually, to die. The activities of certain brain chemicals are also affected. The result is widespread damage to specific brain regions and a decline in abilities affected by those brain regions.
Lewy bodies affect several different brain regions in Lewy body dementia:
- The cerebral cortex, which controls many functions, including information processing, perception, thought, and language
- The limbic cortex, which plays a major role in emotions and behavior
- The hippocampus, which is essential to forming new memories
- The midbrain and basal ganglia, which are involved in movement
- The brain stem, which is important in regulating sleep and maintaining alertness
- Brain regions important in recognizing smells (olfactory pathways)
What are the Causes of Lewy Body Dementia?
The precise cause of Lewy body dementia (LBD) is unknown, but scientists are learning more about its biology and genetics. For example, we know that an accumulation of Lewy bodies is associated with a loss of certain neurons in the brain that produce two important neurotransmitters, chemicals that act as messengers between brain cells. One of these messengers, acetylcholine, is important for memory and learning. The other, dopamine, plays an important role in behavior, cognition, movement, motivation, sleep, and mood.
Scientists are also learning about risk factors for LBD. Age is considered the greatest risk factor. Most people who develop the disorder are over age 50. No specific lifestyle factor has been proven to increase one's risk for LBD.

Other known risk factors for LBD include the following:
- Diseases and health conditions—Certain diseases and health conditions, particularly Parkinson's disease and REM sleep behavior disorder, are linked to a higher risk of LBD.
- Genetics—While having a family member with LBD may increase a person's risk, LBD is not normally considered a genetic disease. Variants in three genes—APOE, SNCA, and GBA—have been associated with an increased risk of dementia with Lewy bodies, but in most cases, the cause is unknown. At this time, no genetic test can accurately predict whether someone will develop LBD, and genetic testing is not usually used in diagnosis. Researchers are looking for more genes that may indicate LBD risk.
What are Lewy Body Dementia Signs and Symptoms?
In this section:
People with Lewy body dementia (LBD) may not have every LBD symptom, and the severity of symptoms can vary greatly from person to person. Throughout the course of the disease, any sudden or major change in functional ability or behavior should be reported to a doctor.
The most common symptoms include changes in cognition, movement, sleep, and behavior.
Cognitive Symptoms of Lewy Body Dementia
LBD causes changes in thinking abilities. These changes may include:
- Dementia—Severe loss of thinking abilities that interferes with a person's capacity to perform daily activities. Dementia is a primary symptom in LBD and usually includes trouble with attention, visual and spatial abilities (judging distance and depth or misidentifying objects), planning, multitasking, problem solving, and reasoning. Unlike in Alzheimer's dementia, memory problems may not be evident at first but often arise as LBD progresses. Dementia can also include changes in mood and behavior, poor judgment, loss of initiative, confusion about time and place, and difficulty with language and numbers.
- Cognitive fluctuations—Unpredictable changes in concentration, attention, alertness, and wakefulness from day to day and sometimes throughout the day. A person with LBD may stare into space for periods of time, seem drowsy and lethargic, or sleep for several hours during the day despite getting enough sleep the night before. His or her flow of ideas may be disorganized, unclear, or illogical at times. The person may seem better one day, then worse the next day. These cognitive fluctuations are common in LBD and may help distinguish it from Alzheimer's disease.
- Hallucinations—Visual hallucinations—seeing things that are not present—occur in up to 80 percent of people with LBD, often early on. They are typically realistic and detailed, such as images of children or animals. Nonvisual hallucinations, such as hearing or smelling things that are not present, are less common than visual ones but may also occur. Hallucinations that are not disruptive may not require treatment. However, if they are frightening or dangerous (for example, if the person attempts to fight a perceived intruder), then a doctor may prescribe medication.
Movement Problems and Lewy Body Dementia
Some people with LBD may not experience significant movement problems for several years. Others may have them early on. At first, movement symptoms, such as a change in handwriting, may be very mild and easily overlooked. Parkinsonism is seen early on in Parkinson's disease dementia but can also develop later on in dementia with Lewy bodies. Specific signs of parkinsonism may include:
Lbd Movie Trailer
- Muscle rigidity or stiffness
- Shuffling walk, slow movement, or frozen stance
- Tremor or shaking, most commonly at rest
- Balance problems and repeated falls
- Stooped posture
- Loss of coordination
- Smaller handwriting than was usual for the person
- Reduced facial expression
- Difficulty swallowing
- A weak voice
Lewy Body Dementia and Sleep
Sleep disorders are common in people with LBD but are often undiagnosed. A sleep specialist can help diagnose and treat sleep disorders. Sleep-related disorders seen in people with LBD may include:
- REM sleep behavior disorder (RBD)—A condition in which a person seems to act out dreams while asleep. It may include vivid dreaming, talking in one's sleep, violent movements, or falling out of bed. RBD may be the earliest symptom of LBD in some people, appearing many years before other LBD symptoms.
- Excessive daytime sleepiness—Sleeping 2 or more hours during the day.
- Insomnia—Difficulty falling or staying asleep, or waking up too early.
- Restless leg syndrome—A condition in which a person, while resting, feels the urge to move his or her legs to stop unpleasant or unusual sensations. Walking or moving usually relieves the discomfort.
Behavioral and Mood Symptoms of Lewy Body Dementia
Changes in behavior and mood are possible in LBD and may worsen as cognition declines. These changes may include:
- Depression—A persistent feeling of sadness, worthlessness, or inability to enjoy activities, often with trouble with sleeping or eating.
- Apathy—A lack of interest in normal daily activities or events; less social interaction.
- Anxiety—Intense apprehension, uncertainty, or fear about a future event or situation. A person may ask the same questions over and over or be angry or fearful when a loved one is not present.
- Agitation—Restlessness, as seen by pacing, hand wringing, an inability to get settled, constant repeating of words or phrases, or irritability.
- Delusions—Strongly held false beliefs or opinions not based on evidence. For example, a person may think his or her spouse is having an affair or that relatives long dead are still living. Capgras syndrome, in which the person believes a relative or friend has been replaced by an imposter, may also appear.
- Paranoia—An extreme, irrational distrust of others, such as suspicion that people are taking or hiding things.
Other Symptoms of Lewy Body Disease
People with LBD can also experience significant changes in the part of the nervous system that regulates automatic functions such as those of the heart, glands, and muscles. The person may have:
- Changes in body temperature
- Problems with blood pressure
- Dizziness
- Fainting
- Sensitivity to heat and cold
- Sexual dysfunction
- A poor sense of smell
Types of Lewy Body Dementia
Lewy body dementia (LBD) refers to either of two related diagnoses—dementia with Lewy bodies (DLB) and Parkinson's disease dementia. Both diagnoses have the same underlying changes in the brain and, over time, people with either diagnosis develop similar symptoms. The difference lies largely in the timing of cognitive (thinking) and movement symptoms. In dementia with Lewy bodies, cognitive symptoms develop within a year of parkinsonism—any condition that involves the types of movement changes, such as tremor or muscle stiffness, seen in Parkinson's disease. In Parkinson's disease dementia, cognitive symptoms develop more than a year after the onset of movement symptoms.
A Diagnosis of Dementia with Lewy Bodies
People with dementia with Lewy bodies have a decline in thinking ability that may look somewhat like Alzheimer's disease. But over time they also develop movement and other distinctive symptoms that suggest dementia with Lewy bodies.
Symptoms that distinguish this form of dementia from others may include:
- Visual hallucinations early in the course of dementia
- Fluctuations in cognitive ability, attention, and alertness
- Slowness of movement, tremor, difficulty walking, or rigidity (parkinsonism)
- REM sleep behavior disorder, in which people physically act out their dreams by yelling, flailing, punching bed partners, and falling out of bed
- More trouble with mental activities such as multitasking and problem solving than with memory early in the course of the disease
A Diagnosis of Parkinson's Disease Dementia
Parkinson's disease dementia starts as a movement disorder, with symptoms such as slowed movement, muscle stiffness, tremor, and a shuffling walk. These symptoms are consistent with a diagnosis of Parkinson's disease. Later on, cognitive symptoms of dementia and changes in mood and behavior may arise.
Not all people with Parkinson's disease develop dementia, and it is difficult to predict who will. Many older people with Parkinson's develop some degree of dementia.
Treatment and Care for Lewy Body Dementia
In this section:
While Lewy body dementia (LBD) currently cannot be prevented or cured, some symptoms may respond to treatment for a period of time. A comprehensive treatment plan may involve medications, physical and other types of therapy, and counseling. Changes to make the home safer, equipment to make everyday tasks easier, and social support are also important.
A skilled care team often can suggest ways to improve quality of life for both people with LBD and their caregivers.
Building a Lewy Body Dementia Care Team
After receiving a diagnosis, a person with LBD may benefit from seeing a neurologist who specializes in dementia and/or movement disorders. A doctor can work with other types of healthcare providers. Depending on an individual's particular symptoms, other professionals may also be helpful:
- Physical therapists can help with movement problems through exercises, gait training, and general physical fitness programs.
- Speech therapists may help with voice volume and projection, and swallowing difficulties.
- Occupational therapists help find ways to more easily carry out everyday activities, such as eating and bathing.
- Music or expressive arts therapists may provide meaningful activities that can reduce anxiety and improve well-being.
- Mental health counselors can help people with LBD and their families learn how to manage difficult emotions and behaviors and plan for the future.
- Palliative care specialists can help improve a person's quality of life by relieving disease symptoms at any stage of illness.
Support groups are another valuable resource for people with LBD and their caregivers. Sharing experiences and tips with others in the same situation can help people find practical solutions to day-to-day challenges and get emotional and social support.
Lewy Body Dementia Medications
Several drugs and other treatments are available to treat LBD symptoms. It is important to work with a knowledgeable health professional because certain medications can make some symptoms worse. Some symptoms can improve with nondrug treatments. Refer to 'Treatment of Behavior and Mood Problems in Lewy Body Dementia.'
Coping with Cognitive Changes
Some medications used to treat Alzheimer's disease also may be used to treat the cognitive symptoms of LBD. These drugs, called cholinesterase inhibitors, act on a chemical in the brain that is important for memory and thinking. They may also improve hallucinations, apathy, and delusions.
The U.S. Food and Drug Administration (FDA) has approved one Alzheimer's drug, rivastigmine (Exelon®), to treat cognitive symptoms in Parkinson's disease dementia. Several other drugs are being tested as possible treatments for LBD symptoms or to disrupt the underlying disease process. Learn more about LBD research.
Kamar, a grandfather of five, was a highly educated executive with a background in the research, development, and field testing of aircraft engines. When he retired at age 67, his wife, Manjit, noticed that he had problems with complex mental activities. He also had trouble with tasks involving a sequence of steps. His doctor prescribed a medication for the cognitive symptoms, which was helpful. Manjit credits the medication for helping Kamar have a better quality of life.
LBD-Related Movement Symptoms
LBD-related movement symptoms may be treated with medications used for Parkinson's disease, called carbidopa-levodopa (Sinemet®, Parcopa®, Stalevo®). These drugs can help make it easier to walk, get out of bed, and move around. However, they cannot stop or reverse the disease itself.
Side effects of this medication can include hallucinations and other psychiatric or behavioral problems. Because of this risk, physicians may recommend not treating mild movement symptoms with medication. If prescribed, carbidopa-levodopa usually begins at a low dose and is increased gradually. Other Parkinson's medications are less commonly used in people with LBD due to a higher frequency of side effects.
A surgical procedure called deep brain stimulation, which can be very effective in treating the movement symptoms of Parkinson's disease, is not recommended for people with LBD because it can result in greater cognitive impairment.
People with LBD may benefit from physical therapy and exercise. Talk with your doctor about what physical activities are best.
Managing Sleep Disorders in Lewy Body Dementia
Sleep problems may increase confusion and behavioral problems in people with LBD and add to a caregiver's burden. A physician can order a sleep study to identify any underlying sleep disorders such as sleep apnea, restless leg syndrome, and REM sleep behavior disorder.
REM sleep behavior disorder, a common LBD symptom, involves acting out one's dreams, leading to lost sleep and even injuries to individuals and their sleep partners. Clonazepam (Klonopin®), a drug used to control seizures and relieve panic attacks, is often effective for the disorder at very low dosages. However, it can have side effects such as dizziness, unsteadiness, and problems with thinking. Melatonin, a naturally occurring hormone used to treat insomnia, may also offer some benefit when taken alone or with clonazepam.
Excessive daytime sleepiness is also common in LBD. If it is severe, a sleep specialist may prescribe a stimulant to help the person stay awake during the day.
Some people with LBD have difficulty falling asleep. If trouble sleeping at night (insomnia) persists, a physician may recommend a prescription medication. It is important to note that treating insomnia and other sleep problems in people with LBD has not been extensively studied, and that treatments may worsen daytime sleepiness and should be used with caution.
Certain sleep problems can be addressed without medications. Increasing daytime exercise or activities and avoiding lengthy or frequent naps can promote better sleep. Avoiding alcohol, caffeine, or chocolate late in the day can help, too. Some over-the-counter medications can also affect sleep, so review all medications and supplements with a physician.
Treatment of Behavior and Mood Problems in Lewy Body Dementia
Behavioral and mood problems in people with LBD can arise from hallucinations, delusions, pain, illness, stress, or anxiety. They may also be the result of frustration, fear, or feeling overwhelmed. The person may resist care or lash out verbally or physically.
Caregivers can try a variety of strategies to handle such challenging behaviors. Some behavioral problems can be managed by making changes in the person's environment and/or treating medical conditions. Other problems may require medication.

Medications are appropriate if the behavior interferes with the person's care or the safety of the person or others. If medication is used, then the lowest possible dose for the shortest period of time is recommended.
The first step is to visit a doctor to see if a medical condition unrelated to LBD is causing the problem. Injuries, fever, urinary tract or pulmonary infections, pressure ulcers (bed sores), and constipation can worsen behavioral problems and increase confusion.
Certain medications, such as anticholingerics and antihistamines like Benadryl®, may also cause behavioral problems. For example, some medications for sleep problems, pain, bladder control, and LBD-related movement symptoms can cause confusion, agitation, hallucinations, and delusions. Similarly, some anti-anxiety medicines can actually increase anxiety in people with LBD. Review your medications with your doctor to determine if any changes are needed.
Not all behavioral problems are caused by illness or medication. A person's surroundings—including levels of stimulation or stress, lighting, daily routines, and relationships—can lead to behavior issues. Caregivers can alter the home environment to try to minimize anxiety and stress for the person with LBD. In general, people with LBD benefit from having simple tasks, consistent schedules, regular exercise, and adequate sleep. Large crowds or overly stimulating environments can increase confusion and anxiety.
Hallucinations and delusions are among the biggest challenges for LBD caregivers. The person with LBD may not understand or accept that the hallucinations are not real and may become agitated or anxious. Instead of arguing, caregivers can help by responding to the fears expressed. By tuning in to the person's emotions, caregivers can offer empathy and concern, maintain the person's dignity, and limit further tension.
Cholinesterase inhibitors may reduce hallucinations and other psychiatric symptoms of LBD, but they may have side effects, such as nausea, and are not always effective. However, they can be a good first choice to treat behavioral symptoms. Cholinesterase inhibitors do not affect behavior immediately, so they should be considered part of a long-term strategy.
Antidepressants can be used to treat depression and anxiety, which are common in LBD. Many of them are often well tolerated by people with LBD.
In some cases, antipsychotic medications are necessary to treat LBD-related behavioral symptoms to improve the quality of life and safety of the person with LBD and his or her caregiver. These types of medications must be used with caution because they can cause severe side effects and can worsen movement symptoms.
If antipsychotics are prescribed, many experts prefer quetiapine (Seroquel®) or clozapine (Clozaril®, FazaClo®), which are types of atypical antipsychotics, to control difficult behavioral symptoms. A newer drug, pimavanserin (Nuplazid®), has been approved by the FDA to treat hallucinations and delusions associated with Parkinson's disease psychosis. However, several serious side effects have been reported, and the FDA requires the same black-box warning for Nuplazid® as it requires for other antipsychotic drugs in the elderly. We do not know yet whether pimavanserin will be helpful in other types of dementia-related psychoses, including LBD. Other potential treatments are being tested.
Typical (or traditional) antipsychotics, such as haloperidol (Haldol®), generally should not be prescribed for people with LBD. They can cause dangerous side effects.
People with LBD may have severe reactions to or side effects from antipsychotics, medications used to treat hallucinations, delusions, or agitation. These side effects include increased confusion, worsened parkinsonism, extreme sleepiness, and low blood pressure that can result in fainting (orthostatic hypotension). Caregivers should contact the doctor if these side effects continue after a few days.
Some antipsychotics, including olanzapine (Zyprexa®) and risperidone (Risperdal®), should be avoided, if possible, because they are more likely than others to cause serious side effects.
In rare cases, a potentially deadly condition called neuroleptic malignant syndrome can occur. Symptoms of this condition include high fever, muscle rigidity, and muscle tissue breakdown that can lead to kidney failure. Report these symptoms to your doctor immediately.
Antipsychotic medications increase the risk of death in all elderly people with dementia but can be particularly dangerous in those with LBD. Doctors, patients, and family members must weigh the risks of antipsychotic use against the risks of physical harm and distress that may occur as a result of untreated behavioral symptoms.
Other Treatment Considerations
LBD affects the part of the nervous system that regulates automatic actions like blood pressure and digestion. One common symptom is orthostatic hypotension, a drop in blood pressure when standing up that can cause dizziness and fainting. Simple measures such as leg elevation, elastic stockings, and, when recommended by a doctor, increasing salt and fluid intake can help. If these measures are not enough, a doctor may prescribe medication.
Urinary incontinence (loss of bladder control) should be treated cautiously because certain medications for this condition may worsen cognition or increase confusion. Consider seeing a urologist. Constipation can usually be treated by exercise and changes in diet, though laxatives, stool softeners, or other treatment may be necessary.
People with LBD are often sensitive to prescription and over-the-counter medications for other medical conditions. Talk with your doctor about any side effects seen in a person with LBD.
If surgery is planned and the person with LBD is told to stop taking all medications beforehand, ask the doctor to consult the person's neurologist to develop a plan for careful withdrawal. In addition, talk with the anesthesiologist in advance to discuss medication sensitivities and risks unique to LBD. People with LBD who receive certain anesthetics may become confused or delirious and have a sudden, significant decline in functional abilities, which may become permanent.
Depending on the procedure, possible alternatives to general anesthesia may include a spinal or regional block. These methods are less likely to result in confusion after surgery. Caregivers should also discuss the use of strong pain relievers after surgery, since people with LBD can become delirious if these drugs are used too freely.
The use of vitamins and supplements to treat LBD symptoms has not been studied extensively and is not recommended. Vitamins and supplements can be dangerous when taken with other medicines. People with LBD should tell their doctors about every medication they take, including prescription and over-the-counter medicines, vitamins, and supplements.
Lewy Body Dementia Research
There is a great deal to learn about Lewy body dementia (LBD). At a basic level, why does alpha-synuclein accumulate into Lewy bodies, and how do Lewy bodies cause the symptoms of LBD? LBD represents an important link between Alzheimer's, Parkinson's, and other brain disorders, and research into one disease often contributes to a better understanding of the others.
Many avenues of research focus on improving our understanding of LBD. Some researchers are working to identify the specific differences in the brain between dementia with Lewy bodies and Parkinson's disease dementia. Others are looking at the disease's underlying biology, genetics, and environmental risk factors. Still other scientists are trying to identify biomarkers (biological indicators of disease), improve screening tests to aid diagnosis and research new treatments.
Scientists hope that new knowledge about LBD will one day lead to more effective treatments and even ways to cure and prevent the disorder. Until then, researchers need volunteers with and without LBD for clinical studies.
Watch 27 Dresses Full Movie
NIH and other groups help people learn about clinical trials and studies and find research opportunities near them. Visit the following websites for details:
- National Institute on Aging (search using the keyword 'Lewy' or the category 'Related Dementias')

For More Information About Lewy Body Dementia
NIA Alzheimer’s and related Dementias Education and Referral (ADEAR) Center
800-438-4380 (toll-free)
adear@nia.nih.gov
www.nia.nih.gov/alzheimers
The National Institute on Aging’s ADEAR Center offers information and free print publications about Alzheimer’s disease and related dementias for families, caregivers, and health professionals. ADEAR Center staff answer telephone, email, and written requests and make referrals to local and national resources.
Lewy Body Dementia Association
404-935-6444
800-539-9767 (toll-free LBD Caregiver Link)
www.lbda.org
Lbd Movie Theater
Lewy Body Dementia Resource Center
833-LBDLINE (toll free)
norma@lbdny.org
https://lewybodyresourcecenter.org
Mayo Clinic
www.mayoclinic.org/patient-care-and-health-information
MedlinePlus
National Library of Medicine
www.medlineplus.gov
Lbd Movie Poster
Michael J. Fox Foundation for Parkinson's Research
800-708-7644 (toll-free)
www.michaeljfox.org
Parkinson's Foundation
800-473-4636 (toll-free)
helpline@parkinson.org
www.parkinson.org
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Lbd Movie Review
Content reviewed: June 27, 2018